When faced with heart problems, choosing the right treatment can be the difference between full recovery and ongoing complications. Angioplasty vs stent are two popular procedures that restore healthy blood flow and reduce heart attack risk. But how do you decide which is best for your situation?
Each year, thousands undergo these life-saving interventions, yet many remain uncertain about their differences.
Let’s explore how angioplasty vs stents compare, when each is more appropriate, and what you can expect from these cardiac procedures.
| Note: Before any cardiac procedure, various tests may be necessary. For a comprehensive overview, check out our detailed guide on 13 common heart tests. |
What Is Angioplasty?
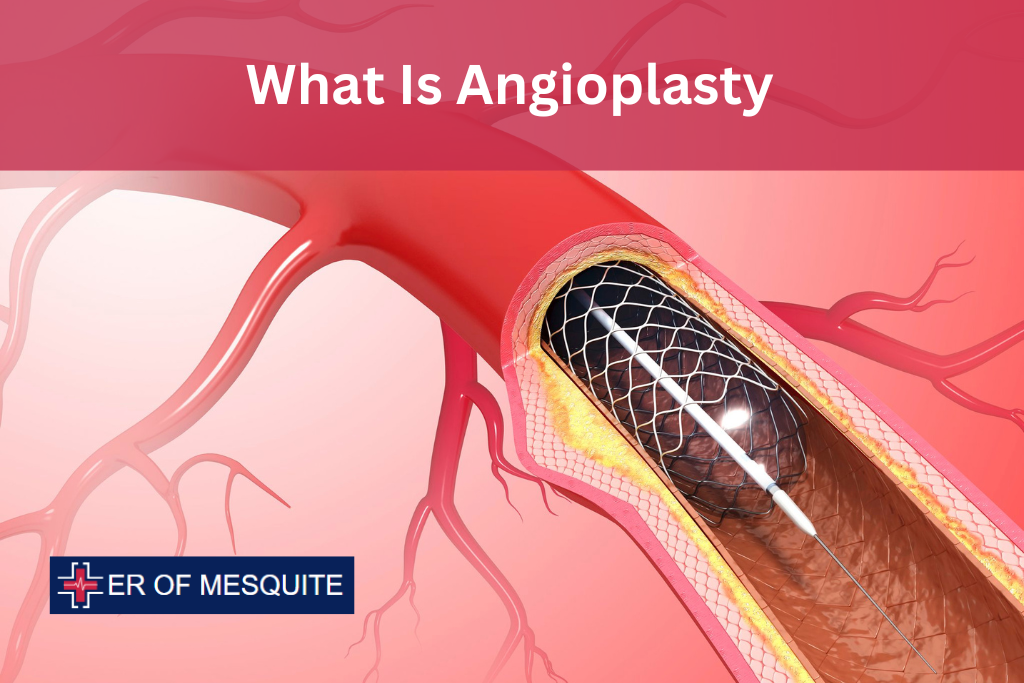
Angioplasty, also known as percutaneous transluminal coronary angioplasty (PTCA), is a minimally invasive procedure designed to open narrowed or blocked blood vessels that supply blood to the heart. The goal of the procedure is to improve blood flow through the arteries, reduce symptoms like chest pain, and minimize the risk of heart attacks.
The procedure typically involves the following steps:
- A catheter (thin, flexible tube) with a small balloon on its tip is inserted into a blood vessel, often in the groin or wrist.
- The catheter is guided through the vascular system to the site of the blockage in the coronary artery.
- Once at the site, the balloon is inflated, pushing the plaque (cholesterol, fat, and other substances) against the artery walls. This widens the artery and restores blood flow.
- After the artery is widened, the balloon is deflated and removed.
Balloon Angioplasty, a specific form of angioplasty, is particularly effective in widening arteries, but there is a risk that the artery may narrow again over time (a condition known as restenosis). To combat this, a stent is often used in combination with angioplasty.
Types of Angioplasty
- Balloon Angioplasty: The most common form of angioplasty, where only the balloon is used to open up the artery.
- Coronary Angioplasty: This is a specific type of angioplasty that targets the coronary arteries, which are the vessels that supply blood to the heart itself.
What Is a Stent?

A stent is a small, metal mesh tube that is inserted into the artery during or after angioplasty to help keep the artery open. It acts as a scaffold, preventing the artery from narrowing again. Stents have significantly reduced the rate of restenosis compared to balloon angioplasty alone.
Stents come in two primary types:
- Bare-metal stents (BMS): These stents are made of metal and serve as a mechanical scaffold to support the artery after angioplasty. While effective, they come with a higher risk of restenosis compared to drug-eluting stents.
- Drug-eluting stents (DES): These stents are coated with medication that is slowly released into the artery to help prevent the growth of scar tissue, further reducing the risk of the artery narrowing again. Drug-eluting stents are considered superior in terms of long-term outcomes, especially for high-risk patients.
Angioplasty vs Stent: Key Differences
While angioplasty vs stents are often discussed together, they are not the same. Here are the primary differences between the two:
Procedure
- Angioplasty: Refers to the balloon procedure that widens the blocked or narrowed artery by pressing plaque against the artery walls. In some cases, angioplasty alone may be sufficient.
- Stent: A stent is typically placed after angioplasty to ensure that the artery remains open. It’s an additional step in the procedure but not always necessary.
Long-term Effectiveness
- Angioplasty Alone: While effective in the short term, balloon angioplasty alone has a higher risk of the artery narrowing again over time.
- Stent Placement: Stents, especially drug-eluting stents, significantly reduce the risk of restenosis and are considered more effective in maintaining long-term artery openness.
Benefits of Angioplasty vs Stents

Both angioplasty and stents offer significant benefits, especially for those suffering from coronary artery disease.
Improved Blood Flow
The most immediate benefit of both angioplasty vs stent is the restoration of normal blood flow through the blocked artery. This improves oxygen delivery to the heart, reducing symptoms like chest pain (angina) and fatigue, and improving overall heart function.
Reduced Risk of Heart Attack
Coronary artery disease is a leading cause of heart attacks. By opening blocked arteries, angioplasty and stent placement can significantly reduce the risk of a heart attack. This is especially true for individuals who have already experienced a heart attack and need to prevent further complications.
Minimally Invasive
Both angioplasty vs stent placement are minimally invasive procedures, meaning they do not require large incisions or open-heart surgery. As a result, recovery time is much faster, with most patients returning to normal activities within a few days or weeks. This is a major advantage over traditional coronary bypass surgery.
Customizable for Patient Needs
Depending on the severity of the blockage and the individual’s health condition, angioplasty can be performed with or without stent placement. For patients with more complex artery blockages, drug-eluting stents provide an added layer of protection against restenosis.
Risks and Complications
While angioplasty and stents are generally safe and effective, there are risks and complications associated with the procedures.
Restenosis
As mentioned, restenosis, or the re-narrowing of the artery, can occur after angioplasty. The use of drug-eluting stents significantly reduces this risk, but it can still happen in some cases. If the artery does narrow again, additional procedures may be required.
Blood Clots
Stents, particularly bare-metal ones, can increase the risk of blood clot formation at the site of placement. This can lead to a heart attack if the clot blocks blood flow. To reduce this risk, patients are typically prescribed blood-thinning medications like aspirin or clopidogrel for a period following the procedure.
Bleeding and Infection
Since angioplasty and stent placement involve inserting catheters through blood vessels, there is a small risk of bleeding, especially at the insertion site (often the groin or wrist). Infection is rare but possible. Careful monitoring and hygiene practices during and after the procedure help minimize these risks.
Allergic Reactions
Some patients may experience an allergic reaction to the materials used in stents, particularly drug-eluting stents, or to the contrast dye used during angioplasty. Inform your doctor if you have a history of allergic reactions to any medications or materials.
Self-Care After Angioplasty or Stent Placement
The success of angioplasty or stent placement doesn’t end with the procedure itself. Self-care plays a critical role in ensuring long-term success and preventing future complications.
Medications
After stent placement, especially with drug-eluting stents, patients are typically prescribed blood thinners to prevent clotting. These medications must be taken exactly as prescribed to prevent complications. Common drugs include aspirin and P2Y12 inhibitors like clopidogrel or ticagrelor.
Lifestyle Changes
Adopting a heart-healthy lifestyle is essential for long-term recovery and overall cardiovascular health. This includes:
- Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limiting salt, sugar, and unhealthy fats can prevent further plaque buildup.
- Regular Exercise: Engaging in moderate physical activity, such as walking or swimming, helps improve cardiovascular health and strengthens the heart muscle.
- Quit Smoking: Smoking is one of the leading causes of coronary artery disease and increases the risk of restenosis. Quitting smoking is crucial for preventing future heart issues.
- Weight Management: Maintaining a healthy weight reduces the strain on the heart and lowers the risk of artery blockages.
Follow-up Appointments
Regular follow-up appointments with your cardiologist are essential to monitor the success of your angioplasty or stent procedure and detect potential complications early. Your doctor may recommend additional tests, such as a Cardiac CT Scan or Angiogram, to assess the condition of your arteries.
At ER of Mesquite, we provide top-quality emergency care that prioritizes your health and well-being. Our offerings also include 24/7 urgent service for heart attack treatment, so you can trust us to be there for you in any emergency situation.