A “broken back” is another term to describe a spinal fracture — a break in one or more vertebrae, the 33 bones that form your backbone and protect your spinal cord. A broken back injury can be worrying, but it doesn’t necessarily mean that there’s damage to the spinal cord.
A bad fall is the most common cause of a broken back. A traumatic injury from a car accident or other collision may also result in a spinal fracture. But other conditions, such as osteoporosis (weak or brittle bones) and spinal tumors, can also lead to vertebral fractures.
A bacterial or fungal infection of the vertebrae may weaken the bones enough to cause a fracture.
What is a Compression Fracture?
Compression fractures are small breaks or cracks in the vertebrae (the bones that comprise your spinal column). The breaks happen in the vertebral body, which is the thick, rounded part on the front of each vertebra. Fractures in the bone cause the spine to weaken and collapse. Over time, these fractures affect posture. The spine curves forward and the person looks “hunched over” (kyphosis).
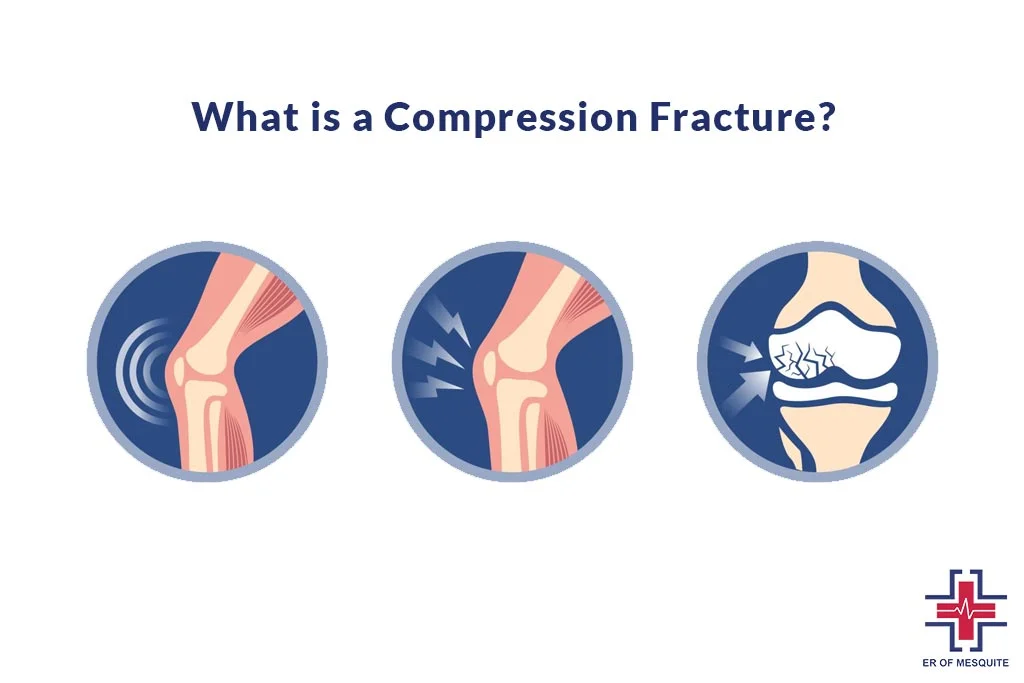
Compression fractures usually happen in the thoracic (middle) part of the spine, especially in the lower thoracic area. Providers also call them vertebral compression fractures (VCF). They often result from osteoporosis. But they can also happen after trauma (such as a car crash) or as a result of tumors on the spine.
Providers treat compression fractures with medications and a special type of back brace. Some people require a minimally invasive procedure to strengthen the vertebrae and stabilize their spine.
What is Spinal Compression Fracture?
It’s easy to think back pain is just part of getting older. But be careful. If you’re nearing age 60, it may be a sign that you have tiny cracks in the bones called vertebrae that form your spine. When these small hairline fractures add up, they can eventually cause a vertebra to collapse, which is called a spinal compression fracture.
Who is At Risk For a Compression Fracture?
Osteoporosis is the most common cause of compression fractures. Preventing and treating osteoporosis is the best way to decrease your risk for compression fractures. Most compression fractures linked to osteoporosis are found in women, especially after menopause. But older men develop osteoporosis and compression fractures, too.
People who have had one compression fracture related to osteoporosis are at a higher-than-average risk of having another one.
How Common Are Compression Fractures?
Compression fractures are common. Almost 1 million compression fractures happen every year in the United States. These spine fractures are more common in older women with osteoporosis (a condition that causes bones to become weak and brittle). They also happen in older men.
Providers estimate that 1 in 4 women over 50 years old have at least one compression fracture. They’re more likely to happen in women who’ve been through menopause. Nearly half of all people over 80 have had a compression fracture.
Compression Deformity vs Fracture
Vertebral compression fractures (VCFs) occur when the bony block or vertebral body in the spine collapses, leading to severe pain, deformity, and loss of height. These fractures more commonly occur in the thoracic spine (the middle portion of the spine), especially in the lower part. On the other hand Compression fractures are small breaks or cracks in the vertebrae (the bones that make up your spinal column). The breaks happen in the vertebral body, which is the thick, rounded part on the front of each vertebra.
What Causes Compression Fractures?
Most compression fractures result from osteoporosis. Bones naturally weaken with age. The vertebrae in the spine become flatter and narrower. Weakened bones are more likely to fracture.

If you have moderate osteoporosis, you might get a compression fracture from a fall or another type of accident. People who have severe osteoporosis can fracture a bone during daily activities. These can include getting out of a car, sneezing, coughing, or twisting suddenly.
In younger people who don’t have osteoporosis, compression fractures usually result from trauma (such as a car accident) or cancer. Cancerous tumors can spread to the spine, weaken the vertebrae, and cause the bones to break.
What Are The Symptoms of Compression Fractures?
The main symptom you’ll notice with a spinal compression fracture is back pain. It may start gradually and get worse over time or come on suddenly and sharply. But regardless of how it happens, it’s important to let your doctor know about it, especially if you’re a woman who is near or over age 50.
Most compression fractures — tiny cracks in the bones of your spine, or vertebra — in women at this age happen because of osteoporosis, a condition defined by bones that are weak and brittle. Treating osteoporosis can help lower your risk for more fractures.
Compression fracture symptoms range from mild to severe. Some people may not have symptoms. Their provider may discover the fracture when they do an X-ray for another condition. But many people are unable to stand or walk without pain. Symptoms of a fractured spine include
- Back pain, which can come on suddenly and last a long time (chronic back pain). It usually develops anywhere between the shoulders and the lower back. Pain usually gets better when you lie down, and it worsens when you stand or walk.
- Decreased mobility or flexibility in the spine. You may not be able to twist or bend over.
- Hunched over appearance (some people call this curved upper back a “dowager’s hump” or hunchback).
- Loss of height as the vertebrae compress and the back curves.
- Pinched nerves and nerve damage, can cause tingling and numbness in the back and difficulty walking.
- Problems controlling the bladder or bowels (these symptoms happen with severe, untreated fractures).
Signs of Multiple Spinal Compression Fracture
When you have multiple spinal compression fractures, your spine will change a lot. Part of your vertebrae may collapse because the cracks mean it can’t support the weight of your spine. That can affect how your body works. Symptoms include
- Height loss. With each fracture of a spinal bone, the spine gets a little bit shorter. Eventually, after several vertebrae have collapsed, you will look noticeably shorter.
- Kyphosis (curved back): When vertebrae collapse, they form a wedge shape, which makes the spine bend forward. Eventually, you’ll have neck and back pain as your body tries to adapt.
- Stomach problems: A shorter spine can compress your stomach, causing digestive problems like constipation, a weak appetite, and weight loss.
- Hip pain: The shorter spine brings your rib cage closer to your hip bones. If those bones are rubbing against each other, it can hurt.
- Breathing problems: If the spine is severely compressed, your lungs may not work properly and you can have trouble breathing.
How To Diagnose Compression Fractures?
For a fracture to be diagnosed, you will need to visit a healthcare provider. Before your doctor can diagnose your condition and design a treatment plan, a complete history and physical examination are necessary. There are many possible internal causes of pain. It is important to determine what is and is not the root of the problem. After the physician has a better idea of what is causing your discomfort, diagnostic tests of some sort may be recommended.
History
First, you will be asked for a complete history of your condition. This may begin by filling out a written form that asks you several questions relating to your pain. The more information you share with your provider, the easier your problem will be to diagnose. Your history is important because it helps your doctor understand: when the pain began, anything that could have caused an injury, physical factors that might be causing the pain, and any family history of similar problems. After reading through your written history, your physician will ask more questions that relate to the information you have given.
Some typical questions include:
- Where do you feel the pain? What is the intensity?
- Does the pain radiate to other parts of the body?
- What factors make the pain feel better or worse?
- Have you had problems with your bladder or bowels?
Physical Examination
After taking your history, the physician will give you a physical examination. This allows the doctor to rule out possible causes of pain and to try to determine what is causing your problem. The areas of your body that will be examined depend upon where you are experiencing pain – neck, lower back, arms, legs, etc. Neurological problems are rare except in younger patients who have experienced a violent injury, such as a car crash.
If a compression fracture is suspected, the doctor will also test for point tenderness near specific vertebrae. Testing specific areas for unusual tenderness allows the doctor to narrow down the cause of your pain.
If a fracture is thought to exist, an X-ray of the spine will generally confirm its presence. An X-ray is a painless process that uses radioactive materials to take pictures of bone. X-rays show bones, but not much soft tissue, so X-rays will be used if fractures are suspected.
If there is a fracture, your doctor may also suggest a CAT scan to make sure that the fracture is stable. The CAT scan is an X-ray test similar to both the MRI and a regular X-ray because it can show both bones and soft tissues. CAT scans are also able to produce X-ray “slices” taken of the spine, so each section can be examined separately. The scan forms a set of cross-sectional images. With a compression fracture, an up-and-down perspective of the spine will be pieced together for examination of stability. The CAT scan is usually done to see if the nerves are in danger from the fracture.
Compression Fracture Treatment
Compression fracture treatment focuses on relieving pain, stabilizing the bones in the spine, and preventing another fracture. Depending on the severity of the fracture and your overall health, treatment may include:
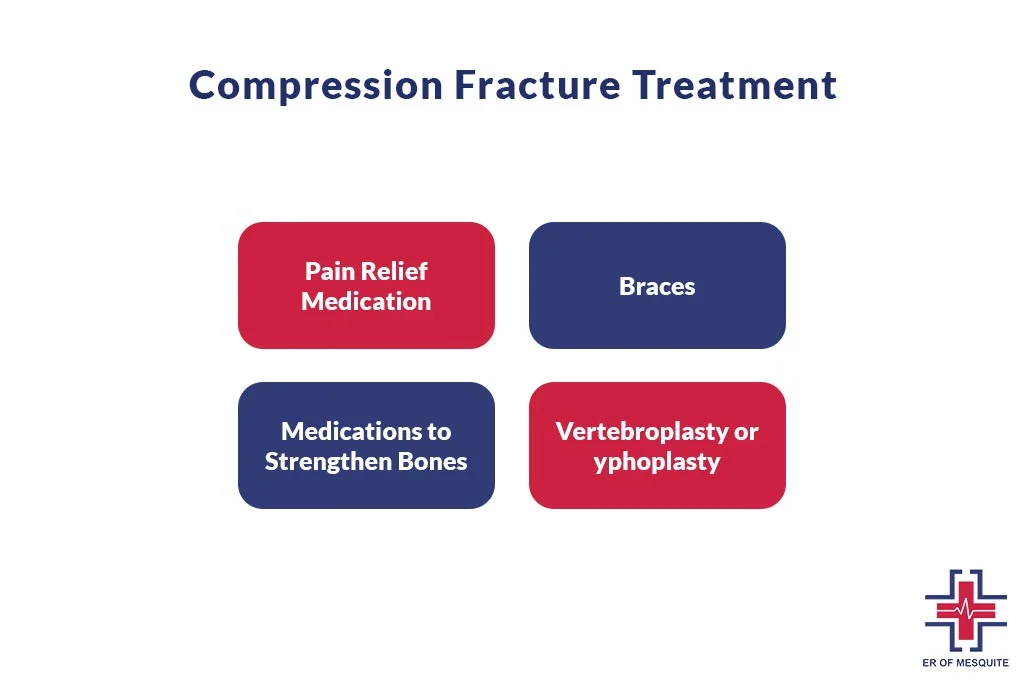
Pain Relief Medication
Your provider may recommend over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs). Or they may prescribe muscle relaxers or prescription drugs. Follow your provider’s instructions carefully when taking these medications.
Braces
A special type of back brace can support your vertebrae. It can also relieve pain by reducing how much you move your spine.
Medications to Strengthen Bones
Drugs called bisphosphonates can slow further bone loss, stabilize the bones, and prevent fractures. These drugs include ibandronic acid (Boniva) and alendronic acid.
Vertebroplasty or Kyphoplasty
These minimally invasive procedures relieve pain, stabilize the bones, and improve mobility. During vertebroplasty, your provider inserts a needle in the vertebra and injects bone cement. During kyphoplasty, they insert an inflatable device that they fill with cement. A vertebroplasty or kyphoplasty is an outpatient procedure, so you’ll go home the same day.
Prevention For Compression Fractures
- You may not always be able to prevent compression fractures. To reduce your risk of a compression fracture from osteoporosis, you should:
- Avoid drinking alcohol excessively.
- Eat a healthy diet and get enough vitamin D and calcium, which strengthen bones.
- Quit smoking and using other tobacco products, since nicotine weakens bones and causes cancer.
- See your provider for regular checkups, and take medications as prescribed to slow bone loss if you’re at risk of osteoporosis.
Long-Term Effects of Spinal Compression Fracture
Two-thirds of spinal compression fractures go undiagnosed because people assume back pain is just a normal part of getting older or that it will resolve on its own. Often, patients don’t seek treatment until multiple compression fractures have occurred.
Possible long-term effects of spinal compression fractures include
- Chronic pain. Over time, multiple fractures can cause the main portion of the vertebrae (the bones that make up the spine) to collapse, causing a great deal of pain and even altering the shape of your spine. In older patients, the chronic pain caused by vertebral compression fractures can lead to a gradual loss of mobility.
- Loss of height. As the spine weakens and changes shape, some people may lose height as their spine becomes shorter.
- Kyphosis. Severe spinal compression fractures may cause a condition called kyphosis. Kyphosis is a forward curvature of the spine that results in a stooped (hunched) posture.
- Patients who experience kyphosis or a similar bending of the spine may also experience symptoms other than back pain. That’s because kyphosis can place additional strain on the body.
In severe cases, regular functions like walking, standing, looking up, and breathing can become strenuous and challenging. Patients with severe kyphosis may also have trouble swallowing and experience acid reflux due to added pressure on the digestive tract.
Best Way to Sleep With a Compression Fracture
Battling a compression fracture doesn’t just test your daytime resolve—it transforms sleep into a tactical mission for comfort. These fractures strain your spine’s sturdiness, disrupting the peace needed for nocturnal healing. Rest isn’t just respite; it’s a critical ally in mending bones. Proper sleep posture, then, isn’t a luxury; it’s a must to dial down pain and keep healing on track. For those nursing a tender back, discovering the sweet spot for slumber can make all the difference. It’s about crafting calm in the night—let’s break down how to achieve that.

Sleeping Positions For Compression Fracture
When a compression fracture is part of your reality, every night invites a quest for the pain-free sanctuary of sleep. The positions you adopt are not mere preferences but strategic choices that can significantly impact your healing journey. Let’s explore the best slumber positions that promote healing while minimizing discomfort:
Stomach Sleeping with Hip Elevation
If you’re a stomach sleeper, tuck a pillow under your hips—not just anywhere, but precisely at waist level. This fine-tunes your spinal alignment, a critical detail that can be the difference between waking up sore or soothed. It’s about creating a subtle lift, a gentle slope that allows your spine to rest without pressure sniping at the fracture.
Remember, each position should be a careful, calculated embrace of rest, ensuring your spine is not just at ease but optimally positioned for healing. It’s like setting the stage for your body to repair under the veil of sleep, night after night.
Back Sleeping with Knee Support
Lying on your back, placing a pillow under your knees. This isn’t just about comfort—it’s a strategic move to preserve your spine’s natural curve and mitigate stress on the fractured site. Imagine your spine like a gently rolling hill—this position keeps that contour intact, making your road to recovery smoother.
Additional Tips For Sleeping With Compression Fractures
Securing a night of restorative sleep with a compression fracture involves more than just choosing the right position—it’s about creating an environment that’s tailor-made for healing. Think of your bedroom as a recovery room where every detail, from the firmness of your mattress to the rhythm of your sleep, is curated to ease your spine into repair. Here are some fine-tuning tips to enhance your sleep environment and quality:
Reinforce with Rigidity
Slipping a bedboard or plywood beneath your mattress isn’t overdoing it—it’s reinforcing your sleep sanctuary. This layer of firmness prevents your spine from diving into softness, which could spell trouble for your fracture.
Pillow Adjustments
Your pillow is not just for your head. Try various sizes and positions—perhaps under your shoulders or lower back—to discover the perfect setup. Each cushion is a tool in your toolkit for the ideal sleep posture.
Pillow Mandotery For Stomach Sleeping
Lying on your stomach without a pillow can arch your back too much. If you must sleep face down, ensure a pillow supports your lower abdomen to keep that spine in check.
Master The Art of Unwinding
Before bed, engage in deep breathing or meditation—think of them as your off-switch from the day’s stressors. These practices aren’t just fluff; they’re potent tools for quieting the mind and coaxing your body into a restful state.
Embrace a Firm Foundation
A firm mattress is non-negotiable; it’s the unsung hero supporting your spine. Envision your mattress as a steady platform, offering a balanced surface that keeps your back aligned and the healing uninterrupted.
Life Expectancy After Compression Fracture
The overall survival rate at 4 years following the VCF was 65.6% for operated patients and 51.9% for those managed conservatively. In the present sample, survival at 4 years was 73.0% for surgically treated patients and 63.0% for those who used a brace.
In severe cases, daily functions like standing, walking, breathing, and turning your head can become a challenge. The long-term effects of compression fractures can seep into everyday life, making it harder to live unassisted or to keep doing the activities you love.
Most compression fractures due to injury heal in 8 to 10 weeks with rest, wearing of a brace, and pain medicines. However, recovery can take much longer if surgery is done. You will lose some height and have a more bent back. Fractures due to osteoporosis often become less painful with rest and pain medicines.
What is The Outlook For People With Compression Fractures
Most people with compression fractures get better without needing medical intervention other than pain relief.
However, older people who experience compression fractures associated with osteoporosis have a higher risk of dying than their peers without osteoporosis. Survival rates are:
- 53.9% at 3 years
- 30.9% at 5 years
- 10.5% at 7 years
Regarding surgery outcomes, one review from 2020 suggests that kyphoplasty and vertebroplasty provide significant pain reduction compared to nonsurgical treatment. Additionally, kyphoplasty tends to result in better restoration of bone height than vertebroplasty.
Conclusion
Compression fractures are most commonly related to weakened bones due to osteoporosis. Other causes include trauma, osteogenesis imperfecta, and tumors spread to the spine from elsewhere in the body. Most people get better with rest and pain relief, but some may require surgery. Doctors can prescribe bisphosphonates to strengthen the bones of people with osteoporosis and help prevent future compression fractures.
Visit the ER of Mesquite for musculoskeletal injuries treatment and talk about your present health. They will provide you with advice on how to cover compression fractures.
