Lyme disease is a noteworthy and frequently misdiagnosed illness in the complicated field of infectious illnesses. Lyme disease, a tick-borne ailment brought on by the bacteria Borrelia burgdorferi, is a rising public health concern as more cases are being reported worldwide. The goal of “Understanding Lyme Disease: A Top-Down Overview” is to help readers better understand this illness by offering a thorough and approachable examination of its epidemiology, symptoms, diagnosis, available treatments, and overall effects on impacted individuals and communities. This overview, which follows a top-down methodology, aims to provide readers with the fundamental knowledge required to appreciate the intricacies of Lyme disease and to facilitate well-informed conversations about its management and prevention.
What is Lyme Disease?
The bacteria that causes Lyme disease is called Borrelia burgdorferi, and it can infect you if a deer tick (also known as a black-legged tick) bites you. The disease is not carried by common “dog ticks” or “wood ticks.”

In 1975, numerous children in Lyme, Connecticut, and two nearby towns were diagnosed with juvenile rheumatoid arthritis, which marked the beginning of the awareness of Lyme disease, also known as borreliosis. Researchers discovered that the arthritis outbreak was caused by bites from infected deer ticks.
What Are The Stages (phases) of Lyme Disease?
Phases or stages of Lyme disease can overlap and result in symptoms affecting the skin, joints, heart, or brain system. These phases consist of:
- Weeks one through four of early localized Lyme illness.
- Lyme disease that spreads early (months one through four).
- Late Lyme illness, late persistent Lyme disease, or simply late Lyme disease (four months or even years later).
Early Lyme Disease
A rash known as erythema migrans typically develops 3–30 days after the virus first manifests itself.
In 70–80% of cases of Lyme disease, the rash appears, and it:
- It usually starts at the site of the tick bite, though it can appear elsewhere as the bacteria spread.
- It usually starts as a small red area that grows over a few days to a diameter of 12 inches, or about 30 centimeters.
- It may lose its color in the center, giving it a bull’s-eye appearance. It is not painful or itchy, but it may feel warm to the touch.
- The rash may or may not show, depending on the skin tone of the affected person.
Later Symptoms of Lyme Disease
It may take months for additional symptoms to appear following a tick bite. Among them are:
- Headaches
- Stiff neck
- More rashes
- Arthritis and joint swelling; muscular, tendon, and bone discomfort; facial palsy—a lack of tone in one or both sides of the face
- Nerve discomfort
- Palpitations, tingling or numbness in the hands or feet, or shooting pains
Without medical intervention, these symptoms might disappear in a few weeks or months. On the other hand, some people experience long-lasting symptoms from chronic Lyme disease.
Without medical intervention, these symptoms might disappear in a few weeks or months. On the other hand, some people experience long-lasting symptoms from chronic Lyme disease.
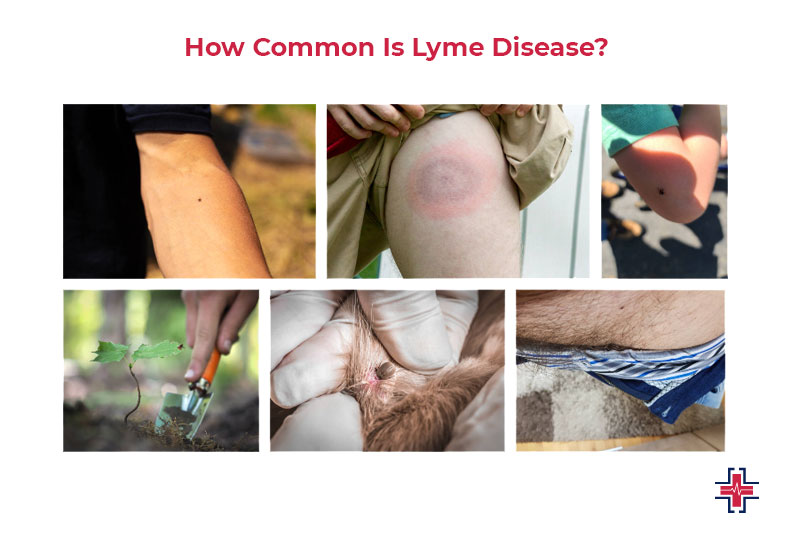
How Common Is Lyme Disease?
The U.S. Centers for Disease Control and Prevention (CDC) receives reports of around 30,000 cases of Lyme disease in the country each year. However, some diagnosed instances remain unreported.
Unusual Symptoms of Lyme Disease
Individuals who have Lyme disease could respond to it differently. The degree of symptoms can vary.
Symptoms of Lyme disease might overlap even though the illness is typically classified into three stages: early localized, early disseminated, and late disseminated. Additionally, some patients may manifest at a later stage of their illness without exhibiting any early warning signs.
- Erythema migraines are a type of reddish rash or skin condition (EM). One week to four weeks after the tick bite, a tiny red patch at the site of the bite marks the beginning of the rash. Over a few days or weeks, the spot enlarges to develop an oval, triangular, or round rash. The rash resembles a bull’s eye because it has a distinct central area surrounded by a red ring. The size of the rash might vary, spanning from the size of a dime to the whole width of the person’s back. Multiple EM rashes (lesions) may develop at various locations on your body as the infection spreads.
- High temperature.
- Ache.
- Rigid neck.
- Aches in the joints and body.
- Tired.
- Enlarged lymph nodes (enlarged glands).
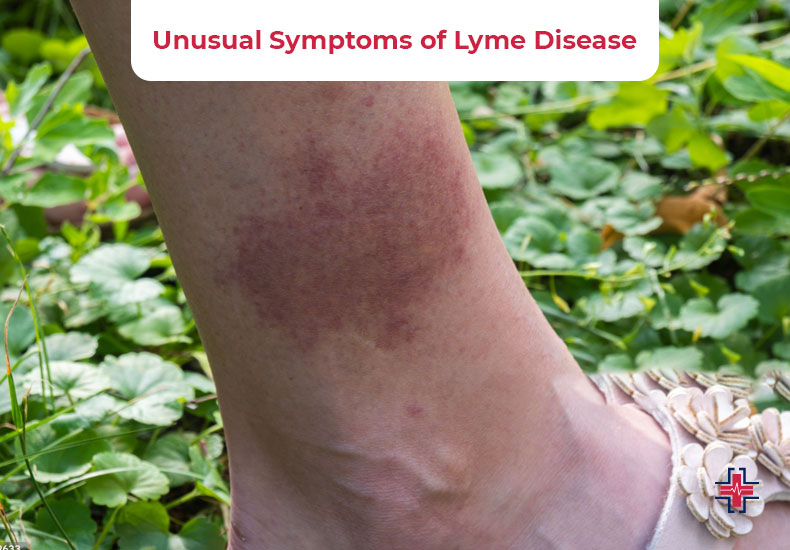
Untreated late Lyme disease can present with any of the following signs and symptoms months to a year after infection:
- Instances of swollen joints that keep happening (arthritis). Usually, this affects the knee and other major joints.
- Confusion is referred to as “brain fog.” This is a type of brain injury known as encephalopathy.
- Damage to nerves throughout the body, encompassing the muscles, organs, and skin (polyneuropathy).
The following are possible indicators and symptoms of the early disseminated stage, or second stage, of Lyme disease:
- Several rash spots.
- Facial muscular paralysis (Bell’s palsy).
- Heart block, or a disruption in the heart’s electrical circuitry.
- Areas affected by altered emotions or numbness (neuropathy).
Signs of Lyme Disease in Kids
The symptoms of Lyme disease in children are typically the same as those in adults.
Typically, they encounter:
- Exhaustion
- Aches in the joints and muscles
- Fever
- Flu-like symptoms
These signs may appear months or years after the infection, or they may appear shortly after.
Your youngster may exhibit some psychological signs. A 2019 analysis found that some parents of children with Lyme disease reported the following psychological problems in their children:
- Rage or hostility
- Mood swings
- Dreams related to depression
Consult our 24 hours urgent pediatric care if these symptoms appear in your child. Also, if they are acting strangely and are unable to articulate the cause or the emotions they are experiencing. Lyme disease is one of the numerous illnesses that could be causing these changes in behavior.
Transmission of Lyme Disease
Any area of your body can become infected with B. burgdorferi-infected ticks. They are more frequently discovered in places of the body that are difficult to notice, like the groin, armpits, and scalp.
For the bacteria to spread, the infected tick has to remain connected to your body for a minimum of 36 hours.
The majority of Lyme disease sufferers were bitten by nymphs or young ticks. Seeing these little ticks is quite challenging. In the spring and summer, they eat. Although they are easier to spot and can be removed before spreading the bacterium, adult ticks are also carriers of the infection.
There is no proof that water, food, or the air may spread Lyme disease. Furthermore, there is no proof that it may be spread via physical contact, kissing, or sexual activity.
Is Person-to-Person Transmission Possible For Lyme Disease?
There isn’t any reliable scientific proof that sexual contact spreads Lyme disease. Published research on animals (Moody 1991; Woodrum 1999) refutes the idea of sexual transmission, and the biology of the spirochete that causes Lyme disease is incompatible with this mode of exposure (Porcella 2001). No proof kissing, caressing, or having sex with someone who has Lyme disease spreads the illness from one person to another. Pregnancy-related untreated Lyme disease can result in placental infection. Although uncommon, spread from mother to fetus is conceivable.
Lyme Disease Pregnancy and Breastfeeding
A few modest studies have connected developmental abnormalities or fetal mortality to Lyme illness during pregnancy. Additional research will be necessary to confirm this.
There haven’t been any reports of breastfeeding-related transmission from a reliable source. Still, a physician might advise against nursing while undergoing treatment. People with Lyme disease require a different kind of medication during pregnancy.
Diagnoses of Lyme Disease
Anyone experiencing a rash that might have been caused by tick exposure must get medical help right once. Be ready to describe the probable exposure. This could be related to say a recent trek in a region where ticks are prevalent.
After removing a tick, one should photograph it and identify the species. It is important to note that Lyme disease patients who do not obtain treatment on time may develop more serious symptoms later on. These may show up years later.
When antibodies are present, some weeks following the first infection, blood tests are most accurate. A medical practitioner may request the following tests:
- The B. burgdorferi antibody assay, or ELISA, is used to find antibodies against the pathogen.
- An ELISA test that is positive is confirmed using a western blot. It looks for antibodies against particular proteins found in B. burgdorferi.
- People who have persistent symptoms of Lyme arthritis or nervous system disorders are evaluated using a polymerase chain reaction (PCR)Trusted Source. Joint fluid or cerebrospinal fluid (CSF) is used for the procedure. Because PCR testing on CSF is not very sensitive, it is not usually advised for the diagnosis of Lyme disease. The diagnosis is not ruled out by a negative test. In contrast, if joint fluid is tested before antibiotic therapy, the majority of patients will have positive PCR results.
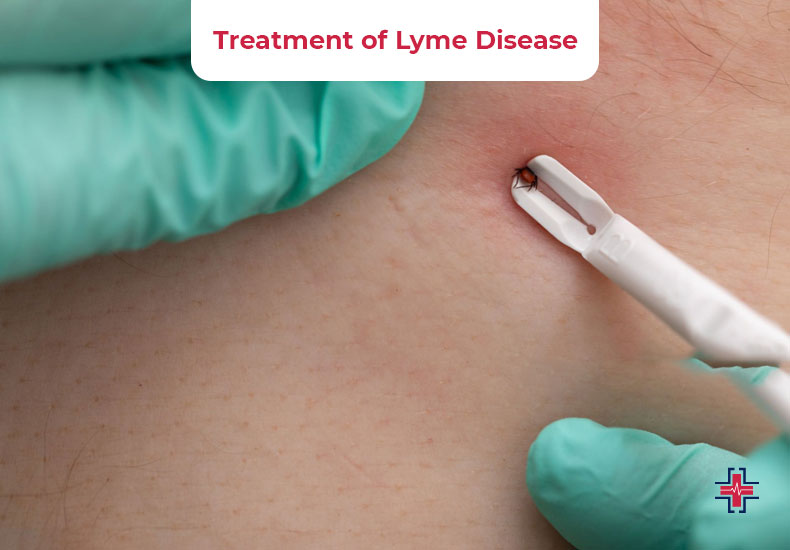
Treatment of Lyme Disease
Early treatment is ideal for Lyme illness. A straightforward 10-14-day course of oral antibiotics is the treatment for early localized disease, which aims to eradicate the infection.
The following drugs are used to treat Lyme disease:’
- Amoxicillin and cefuroxime are medications used to treat nursing mothers.
- Cefuroxime, doxycycline, or amoxicillin are the first-line medications for both adults and children.
Intravenous (IV) antibiotics are used for some kinds of Lyme disease, notably those with cardiac or central nervous system (CNS) involvement.
Healthcare providers will usually go to an oral regimen to complete the course of treatment after improvement. Typically, the entire course of treatment lasts between 14 and 28 days. Lyme disease Oral antibiotics are used to treat, a late-stage Lyme disease symptom that can appear in certain individuals, for 28 days.
What Kind of Doctors Treat Lyme Disease?
You may get a Lyme disease test from any type of doctor. That does not, however, imply that having your podiatrist or dermatologist request the diagnostic tests is a smart idea. Many people only seek a Lyme diagnosis and treatment by visiting their family doctor or primary care physician.
A doctor with extensive expertise treating patients with Lyme disease is known as an LLMD because of their familiarity with the wide range of symptoms, co-infections, and complications that can arise from the disease at different stages. Many patients also find LLMDs to be more understanding and understanding of their experiences because of their knowledge and skill, particularly if they’re having trouble receiving an appropriate diagnosis from another doctor.
- Despite the negative findings of your Lyme disease test, you continue to experience symptoms.
- Even though you have previously had treatment for Lyme disease, the persistence of your symptoms may be a sign of chronic Lyme disease.
- Your symptoms haven’t disappeared despite receiving treatment for common misdiagnoses of Lyme disease, such as rheumatoid arthritis or chronic fatigue syndrome.
- Lyme disease, chronic Lyme disease, and Post-Treatment Lyme Disease Syndrome are not accepted diagnoses by your doctor.
Patients who do not fit into any of the aforementioned categories could nevertheless feel more comfortable leaving their care in the hands of an LLMD who is knowledgeable about the different manifestations of Lyme and other tick-borne illnesses.
Home Remedies for Lyme Disease
To treat Lyme disease, many patients resort to natural therapies. Natural remedies are not considered alternatives or replacements for medical care; rather, they are considered complementary therapies, to be used in conjunction with traditional medications or treatments.
Essential Oils for Chronic Lyme
Many essential oils are thought to have antibacterial properties, which is why some Lyme disease sufferers who have had the disease for a long time have resorted to essential oils to assist in managing their symptoms.
Cinnamon bark, clove bud, citronella, wintergreen, and oregano were found to exhibit strong activity against B. burgdorferi in lab tests conducted on human subjects—even more so than daptomycin, the “gold standard” antibiotic that is often prescribed to patients with Lyme disease.
These findings suggest that essential oils may be useful in treating persistent Lyme illness, but further research is required to demonstrate these benefits in human patients.
Most essential oils are safe and have no negative side effects when used correctly. But it’s crucial to utilize them with caution. Some of them shouldn’t be consumed internally and should be appropriately diluted to avoid irritating the skin.
Using Herbs to Treat Lyme Disease
Herbs have been utilized for thousands of years in medicine. When medications are unable to completely relieve their Lyme disease symptoms, many people resort to natural therapies.
According to one study, using the antibiotic doxycycline with the Chinese skullcap’s active component, baicalein can have significant therapeutic effects. Even more promising, a 2020 lab investigation discovered that seven herbal remedies had anti-B. burgdorferi (Lyme bacteria) action when contrasted with the antibiotics cefuroxime and doxycycline:
- Synanolenta Cryptolepis
- Black walnut, or Juglans nigra
- Cistus incanus
- Japanese knotweed, Polygonum cuspidatum
- A annua, sometimes known as sweet wormwood
- Uncaria tomentosa: the paw of a cat
- Chinese skullcap, Scutellaria baicalensis
The antibacterial characteristics of these plants show promise, but further studies are needed to confirm their usefulness against Lyme disease in humans.
Lyme Disease Rate
According to recent estimates derived from alternative techniques, there may be 476,000 cases of Lyme disease in the US annually. surveillance information.
FAQs
Can You Get Lyme Disease Twice?
It is possible to contract Lyme disease more than once, though, as occasionally the immune system may not create enough antibodies to fully guard against the bacterium. It’s crucial to remember that Lyme disease might recur even if a patient adheres to a suitable treatment plan.
Why Do So Many Celebrities Have Lyme Disease?
Some of our favorite celebrities, sports heroes, political figures, and people in the public eye that we look up to will inevitably have Lyme disease since the chances of them coming into contact with an infectious tick are higher for those who enjoy being outside in the spring and summer.
Do Mosquitoes Carry Lyme Disease?
There is no proof that mosquitoes may transmit the Lyme disease bacterium in the quantity and condition necessary for an illness, even though the germs have been discovered in their salivary glands.
Can Lyme Disease be Sexually Transmitted?
It is not possible for someone to contract Lyme disease by touching, kissing, or sexual contact with an infected person. Pregnancy-related untreated Lyme disease can result in placental infection. Although uncommon, spread from mother to fetus is conceivable.
Can Lyme Disease Cause Seizures?
Seizures may also be brought on by Lyme illness, but the timing of the seizures was associated with the build-up of normeperidine, the primary meperidine metabolite that stimulates the central nervous system.
Summary
In conclusion, developing a comprehensive understanding of Lyme disease is imperative for those navigating its intricacies. This top-down overview has shed light on the causes, symptoms, and treatment options related to Lyme disease. However, early detection through Lyme disease testing is paramount. Individuals concerned about potential exposure or experiencing symptoms should actively seek Lyme disease testing near me to ensure prompt diagnosis.
Equally crucial is connecting with our qualified healthcare professionals at the urgent care Mesquite specializing in Lyme disease, such as Lyme disease doctors near me, for accurate assessment and tailored treatment plans. By staying informed, proactive, and utilizing nearby testing facilities and specialized physicians, individuals can enhance their ability to effectively manage Lyme disease, emphasizing the importance of timely intervention for optimal health outcomes.